
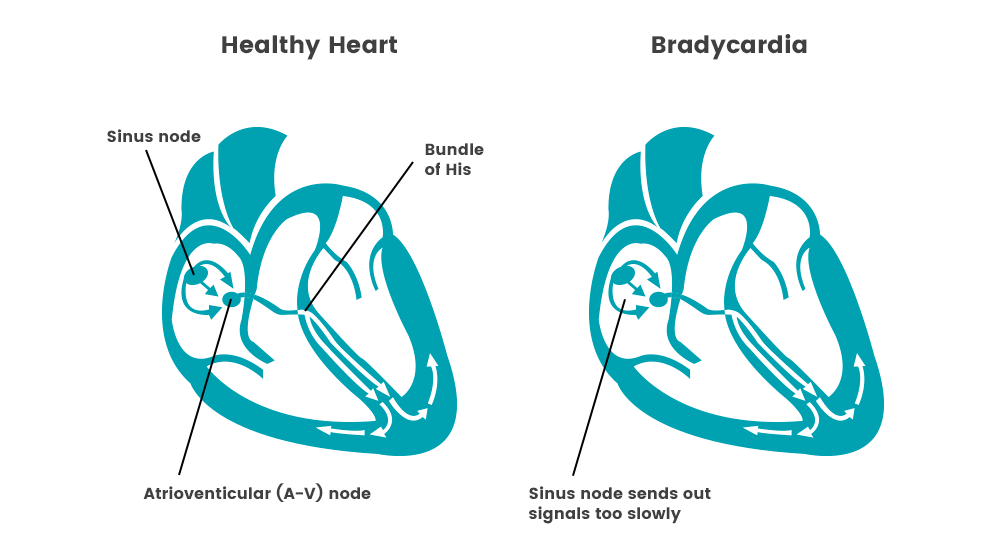
Bradycardia can be caused by numerous factors, including heart tissue damage related to aging, heart disorder present at birth, underactive thyroid gland, inflammatory disease, medications, damage to heart tissues from heart disease or heart attack, or repeated disruption of breathing during sleep.
The sinus node in the heart acts as a natural pacemaker, and this is most often where bradycardia starts. A slow heart rate might occur because the sinus node discharges electrical impulses slower than normal, pauses or fails to discharge at a regular rate, or discharges an electrical impulse that is blocked before it can cause the atria to contract. Other times, bradycardia can be caused when the electrical signals transmitted through the atria aren’t transmitted to the ventricles (heart block or atrioventicular block).

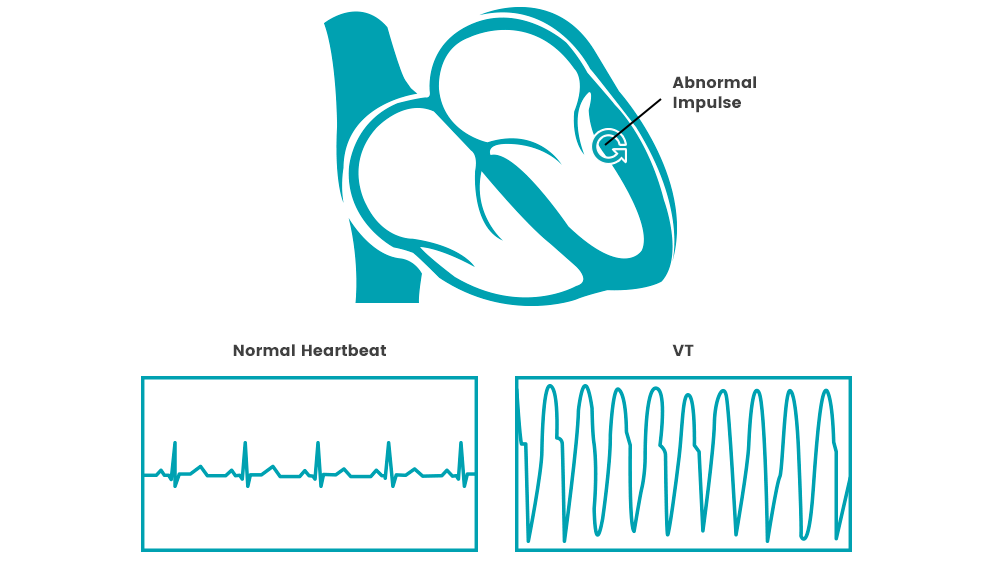
Symptoms of sudden cardiac arrest are immediate and drastic and include no pulse, no breathing, loss of consciousness and sudden collapse. There are often other symptoms that precede sudden cardiac arrest and could include fatigue, shortness of breath, dizziness, weakness, vomiting, blackouts, and more. However, most often, there are no warning signs.
When sudden cardiac arrest occurs, the lack of oxygenated blood can cause brain damage in only a few minutes. Death or permanent brain damage can occur within four to six minutes, so immediate action is necessary as timing is critical.
Sudden cardiac arrest occurs when your heart suddenly starts beating very fast and irregular, quivering instead of pumping. The body and brain are deprived of oxygen during this type of arrhythmia. If you are at risk, an implantable defibrillator can treat these dangerous fast heart. If this type of arrhythmia is untreated, it can cause death in minutes. Sudden cardiac arrest is caused by an electrical issue in the heart which causes the heart to quiver, rather than pump blood. People who experience sudden cardiac arrest typically lose consciousness before they can alert anyone about their symptoms
Sudden cardiac arrest is most often linked with coronary artery disease, making the risk factors very similar. These factors include a family history of coronary artery disease, obesity, diabetes, a sedentary lifestyle, heavy alcohol consumption, high blood pressure and/or cholesterol, and smoking. Other factors include a previous heart attack or cardiac arrest episode, age, family history of other forms of heart disease, use of illegal drugs, and nutritional imbalance.
While there’s no way to know your risk for sudden cardiac arrest, you can take measures to decrease your risk. Simple steps to take include making sure you are physically active, eating a nutritious and balanced diet, and limiting alcohol consumption. If you know you have a greater risk for heart disease or have an unhealthy heart, your doctor could recommend taking medications to improve your health. If some cases with a known high risk of sudden cardiac arrest, doctors may recommend anti-arrhythmic drugs or an implantable cardioverter-defibrillator (ICD) as primary prevention.